The retina consists of ten distinct layers. Rather than simply memorizing their names, understanding how each layer connects by drawing schematic diagrams is key. This foundational knowledge helps interpret a wide range of ocular diseases and imaging findings, especially in early stages of training.
Overview of the 10 Retinal Layers and Their OCT Correlates
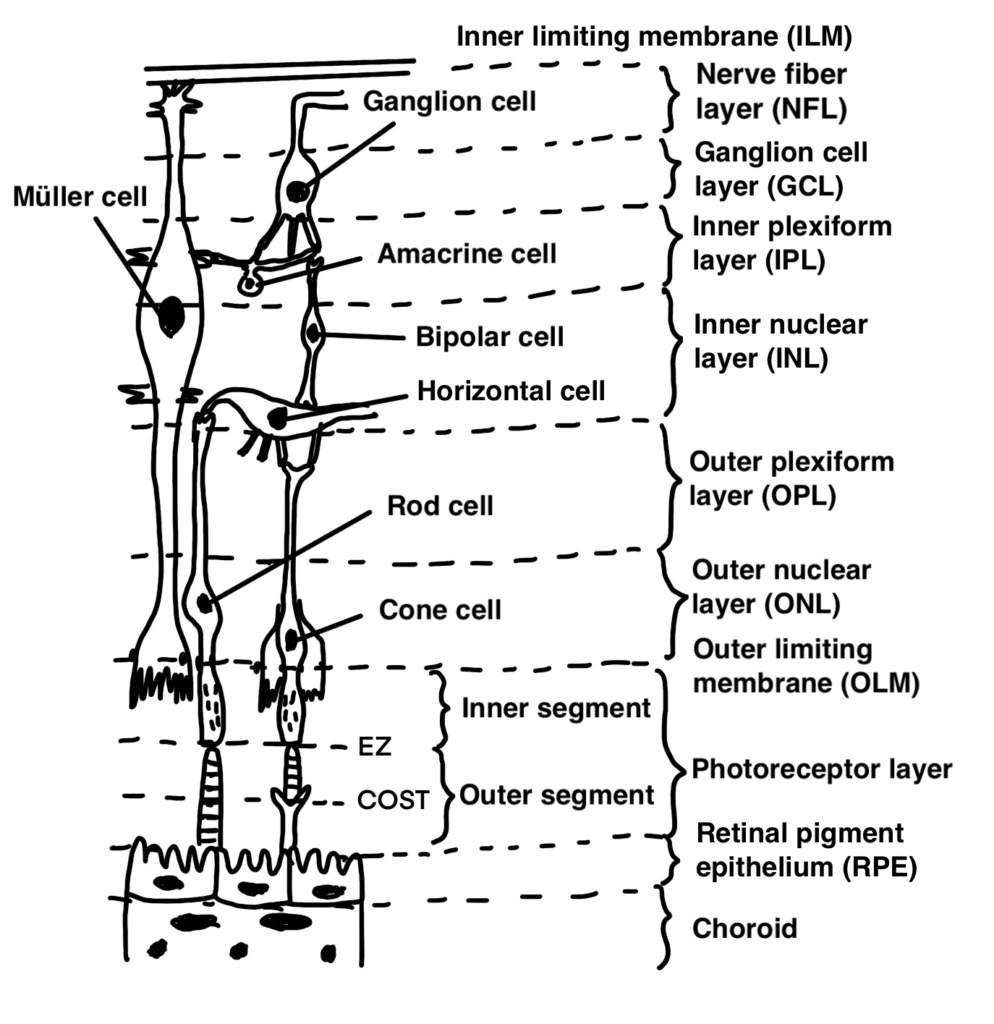
Refer to the schematic diagram provided above. It illustrates the general structure of the ten retinal layers.
In clinical practice, when reading OCT images, it’s not enough to look passively. If you interpret the images with a solid understanding of retinal anatomy and pathophysiology, the amount of useful information you can extract increases dramatically.
Example 1: Glaucoma
Glaucoma is a disease in which retinal ganglion cells are damaged, leading to progressive visual field loss. On OCT, this is evaluated by measuring the thickness of the GCC (Ganglion Cell Complex), which includes:
- Nerve fiber layer (NFL)
- Ganglion cell layer (GCL)
- Inner plexiform layer (IPL)
As the schematic shows, ganglion cells span these three layers, making the GCC a meaningful biomarker in glaucoma diagnosis and monitoring.
Example 2: Central Retinal Artery Occlusion (CRAO)
In the acute phase of CRAO, ischemia leads to cytotoxic edema of the ganglion cells. On OCT, you will notice swelling specifically localized to the layers where ganglion cells reside.
Example 3: Rhegmatogenous Retinal Detachment (RRD)
When a retinal detachment involves the macula, visual acuity often decreases.
However, macular detachment alone does not always lead to visual impairment.
In cases like central serous chorioretinopathy (CSC), patients may have submacular detachment yet maintain a best-corrected visual acuity of 1.0.
So why does vision drop in RRD? The answer lies in damage to the outer nuclear layer (ONL). This layer contains the nuclei of rod and cone photoreceptors, and disruption here leads to permanent visual loss. Indeed, several studies have shown that ONL thickness correlates with visual prognosis following detachment.
In contrast, in CSC, the ONL and retinal architecture are typically preserved, which explains why visual acuity remains intact despite serous retinal detachment.
What is the Foveal Bulge?
Looking at the schematic, you’ll notice that cone cells are typically shorter than rod cells.
However, the cones located at the fovea are structurally unique. They resemble rods and are referred to as rod-like cones. Because of this, the Ellipsoid Zone (EZ) shows a slight central bulge at the fovea, known as the foveal bulge.
Interestingly, in conditions such as CSC or retinal vein occlusion (RVO), even after treatment when the EZ appears intact and the overall retinal structure is restored, some patients still report poor visual recovery. In these cases, the foveal bulge may be absent, suggesting subtle photoreceptor damage not evident on routine scans.